The Secondary Billing feature enables you to bill secondary claims and informs you when secondary claims are ready to be batched. Most secondary claims are created using this batch method. Secondary claims are necessary to apply a secondary payment. The patient's responsibility is transferred from the primary insurance to the patient’s secondary insurance. This process is known as coordination of benefits (COB).
How do I set up my practice to automatically batch secondary and crossover claims?
Set up your practice to automatically create secondary claims by activating the Auto Create COB setting in Administration: Practice Information. When you activate this setting, secondary and crossover claims are batched overnight from those eligible in the Secondary Billing worklist.
How do I manually create a secondary claim?
For instructions, refer to Secondary Claims.
Requirements for Claims to Appear in Secondary Billing
- A secondary payer must be present on the primary claim or there is an active secondary payer profile in the patient chart.
- If the patient has an active secondary payer profile in the chart, the claim will appear in Secondary Billing.
- The primary claim must be finalized with a $0 insurance balance within the last 180 days. The primary insurance payment and/or adjustments have been successfully applied to the entire claim.
- There must be an outstanding patient responsibility that is reporting in the patient's A/R.
- The most recent primary claim is not marked for appeal.
- Claim/charge does not have a secondary claim already created.
- Claim/charge has not been excluded from the worklist.
- Patient responsibility has not been written off.
Notes
- Creating the secondary claim prior to finalizing the primary claim (applying payment and/or adjustments) may result in an inaccurate AR. Secondary billing is recommended prior to generating patient statements.
- We recommend archiving or marking ancillary profiles, such as DMERC, as tertiary payers to prevent any problems.
Secondary Claim Types
| Type | Description |
|---|
| Electronic | Electronically transmitted along with the payment and adjustment information posted from the primary claim. It is not necessary to send a paper copy of the EOB. If an electronic payer does not support an electronic secondary claim, select the print locally option. |
| Paper | Printed locally on a CMS-1500 form. We recommend that you attach a copy of the primary EOB to the form. |
| Crossover | When Medicare is the primary insurance, it will likely crossover the primary claim to the secondary payer. NextGen® Office does not transmit crossover claims to the payer. |
Open Secondary Billing
From the Billing menu, select Secondary Billing.
Secondary Billing Overview
There are two tabs on this page:
Filters
| Filters | Description |
|---|
| Filter the view | All claims appear by default. The other view option is crossover claims. |
| Primary Payer | The primary payer in the patient's chart |
| Patient | Filter by a specific patient |
| Sort by Column | You can sort by the following columns in either ascending or descending order:
- Date of service
- Claim charge amount
- Primary Payer
- Secondary Payer
|
| Payer | The secondary payer in to the patient's chart |
| Service Date | Date of service when the claim was created |
Columns
| Column Name | Description |
|---|
| Claim ID | Lists all primary claims with finalized status within the last 180 days |
| Service | Date of service when the claim was created |
| Patient Name | Patient's name |
| Charges | Outstanding patient responsibility that appears in the patient's A/R |
| Primary Payer | The payer to whom the primary claim was sent |
| Crossover Payer | The primary payer automatically forwards the claim to this payer |
| Secondary Payer | The secondary payer listed in the primary claim.
Note: If this column is blank, it means that a secondary payer was added to the patient's chart after the primary claim was created. |
Primary Claims
The Primary Claims tab shows a list of all primary claims that require a secondary claim.
Select one or more claims and select one of the following four Secondary Billing functions:
Create Secondary
Use this option to create a COB claim electronically or using paper. If the payer does not offer electronic claim option, choose paper. If COB claim payer uses paper, you must print the claim locally on a CMS-1500 form and mail it to the payer. We recommended that you attach a copy of the primary EOB.
- Select the check box next to the claim ID and click Create Secondary.
The claim moves to the Batch Status tab in queued status. Once the claim is created, the status changes to ready.
- Click the Date link to view the secondary claim details.
Shift Crossover Balance to Secondary
A crossover payer is listed under the
Crossover Payer column if a primary payer automatically forwarded the primary claim to the secondary insurance. This option is used if the primary payer is Medicare. A crossover claim must be created to:
- Post a secondary ERA or EOB once processed by the secondary payer.
- Move the patient balance to the insurance balance.
Note: Once crossover claims are created, they are not batched out with the other claims. Since the claim was already sent to the secondary payer, we will not be transmitting another claim as it would be a duplicate. These claims do not leave the system.
- Select the check box next to the claim ID and click Shift Crossover Balance to Secondary.
The claim moves to the Batch Status tab in queued status. Once the claim is created, the status changes to ready.
- Click the Date link to view the crossover claim details.
Write-off Patient Balance
This option enables you to write off the patient’s responsibility from the secondary claim when you choose not to bill the secondary payer.
- Select the check box next to the claim ID and click Write Off Patient Balance.
The claim moves to the Batch Status tab in queued status. Once the write-off is successful, the status changes to ready.
- Click the Date link to view the list of successful write-offs for that date.
- Click the Claim ID link to view the payment details.
Remove from Work List
This option enables you to remove the claim from the Secondary Billing worklist for any reason without creating a COB claim. Select the check box next to the claim ID and click Remove From Work List.
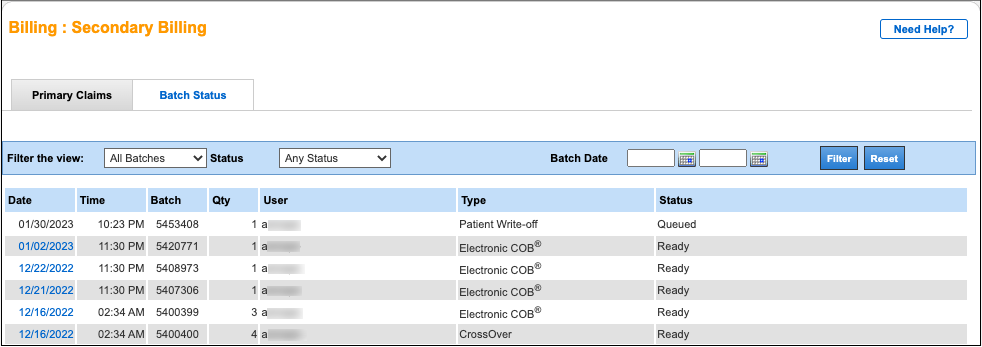
Batch Status
After the Create Secondary or Shift Crossover Balance to Secondary function is processed, the claims are moved to the Batch Status tab with queued status until the system creates the secondary claim. Depending on the number of claims, the batch may be queued for up to ten minutes. After the claim is successfully created, the status changes to ready. All secondary claims will batch out with all other claims at the end of the day.
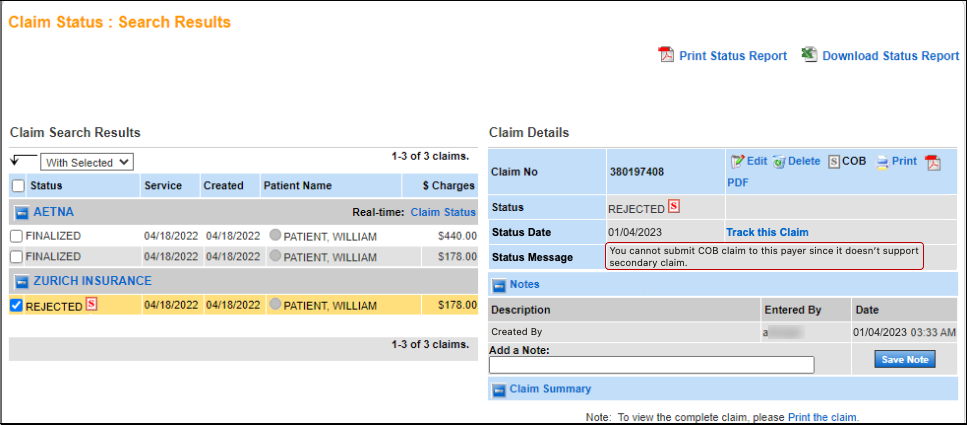
Once the batch status changes to ready, click the date to view the batch of secondary claim details. If secondary claims are rejected, additional information may be required.
Electronic payers that do not support secondary electronic claims are rejected with the status message as shown below. Edit and submit the claim on paper.
Note: If the claims are sent electronically, the EOB does not have to be attached. For paper claims, the EOB should be attached.
See Also: Administration: Practice InformationSecondary Claims


