This article describes how to create a single secondary claim. The majority of secondary claims should be created using our Secondary Billing batch option. If a secondary claim is not created, the patient will have a balance from the primary claim. After the secondary claim is created, the patient’s balance from the primary claim is transferred to the secondary payer’s insurance balance. This process is known as coordination of benefits (COB).
Note: Do not submit a secondary claim until you have received payment from the primary insurance. Creating a secondary claim before finalizing the primary claim may result in inaccurate AR.
Requirements for Creating a Secondary Claim
- The primary claim must be in finalized status for the COB option to be enabled. This function prefills all primary payment and adjustment information for the secondary payer to review. This information is based on the same information available on the EOB or ERA.
- Each service line must be balanced to $0.00 in the charge ledger.
- If the secondary payer was not on the primary claim, this information must be manually added in the secondary claim form.
Types of secondary claims
- Electronic: This is electronically transmitted along with the payment and adjustment information posted from the primary claim. It is not necessary to send a paper copy of the EOB. If an electronic payer does not support an electronic secondary claim, select the Print Locally option.
- Paper: Must be printed locally on a CMS-1500 form. We recommend that you attach a copy of the primary EOB to the form.
- Crossover: When Medicare is the primary insurance, Medicare will likely crossover the primary claim to the secondary payer. NextGen Office does not transmit crossover claims to the payer.
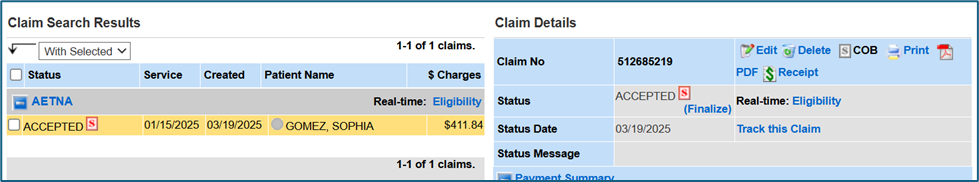
Create a Single Secondary Claim
- Review the Requirements for Creating a Secondary Claim first
- Go to the Patient’s chart > select Claim History
- Locate the Primary Payer and the Date of Service (claim should be in finalized status)
- Select COB

- The secondary claim screen displays mimicking a CMS-1500 form.
- Select the secondary payer from the drop-down list, type the Patient’s last name in the search box, and click search.
- Select the insurance ID number displayed for the secondary payer. This step will populate all the relative patient information into the fields required for the secondary claim.
- Additionally, if the primary charge was properly balanced, all the required primary payment information will automatically populate into the appropriate fields and the claim can be submitted without any additional steps.
- Scroll to the bottom and click Submit.
- The secondary claim has been created and sent to HF Accepted.
Note: If the secondary claim will not create, review the error messages and corresponding boxes. This may require a examination of the original primary payment posting.
See Also
Last Update: 3/22/25



