Attestation Portal
Submit performance data in the Quality Payment Program (QPP) attestation portal using Quality measure QRDA files and Promoting Interoperability measures from My Reports.
Date CMS Submission Window Opens for 2021 Performance Year
January 3, 2022
2022 Performance Year Deadline
- March 31, 2023 8:00 PM EDT: Attestation deadline for Medicare’s MIPS Quality and Promoting Interoperability Programs
- Medicaid Promoting Interoperability Program attestation deadlines vary by state. Confirm the deadline with your state Medicaid agency.
Flexibilities for Clinicians Participating in MIPS in 2022 Because of the COVID-19 (Novel Coronavirus) Public Health Emergency
Clinicians significantly affected by the public health emergency may submit an Extreme and Uncontrollable Circumstances Application to reweight any or all of the MIPS performance categories. Applicants must provide justification of how their practice has been significantly impacted by the public health emergency.
Information about QPP Exceptions
About QPP Exceptions
Information about QPP's COVID-19 Response
Quality Payment Program COVID-19 Response
EHR Certification ID
0015ELC7MG7SV5Y
EHR Vendor Letter (or CEHRT Letter) for Medicaid Attestation
Contact NextGen Office Client Support at 877-523-2120 or 858-523-2120, option 6, sub-option 4.
Export Quality Measure QRDA Files
Export Promoting Interoperability Measures
- Export the Excel file within Report Card Export in My Reports.
- Enter the numerator and denominator values in the attestation portal.
Quality Measures
How do you know which Quality measures to select? Should you select the six measures with the highest passing rates?
If you select the top six measures based on the passing rates on the MIPS Dashboard you may be negatively impacting your scoring results.
NextGen Office only presents the QRDA performance and passing rates. The benchmarks applied by the Quality Payment Program is the missing piece.
Benchmarks and Deciles
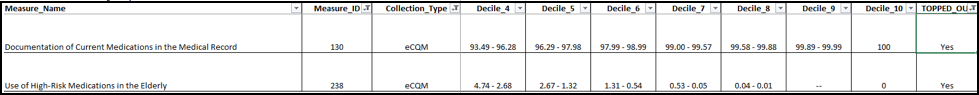
CMS benchmarks show that Use of High-Risk Medications in the Elderly and Documentation of Current Medications in the Medical Record measures as topped out, which means the maximum achievable number of points is 7.
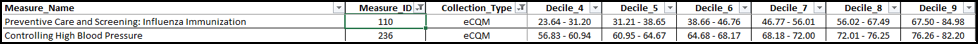
In the example below, the Preventive Care and Screening: Influenza Immunization and Controlling High Blood Pressure measures show scores in the high 70s based on the benchmarks. However, these measures are in decile 9 and need to be included to ensure maximum scoring results.
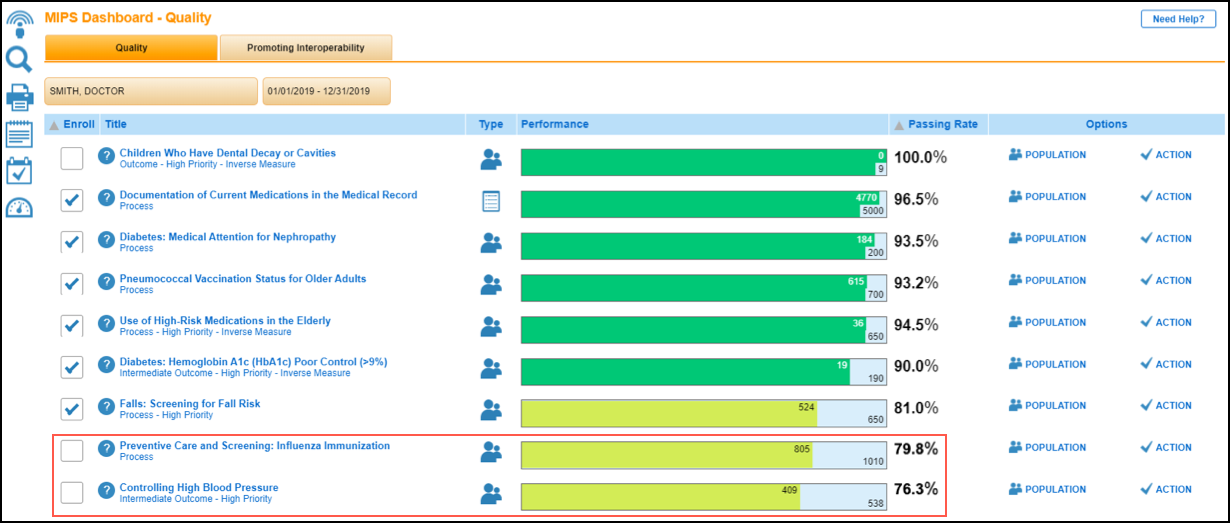
There is no negative impact to your incentive payment results for submitting extra measures. It will instead ensure that you are receiving the best score possible.
Note: All measures submitted will be published on public repositories such as Data.Medicare.Gov.
Where to Access the Benchmarks
- Go to the Quality Payment Program Quality Measures page.
- Click 2022 Quality Benchmarks to download the ZIP file.
In Case of Audits
Retain a copy of all submitted reports (available in My Reports) to ensure you can provide all necessary documentation during an audit.
NextGen Office Resources
Export QRDA I and QRDA III Files2022 MIPS Readiness Checklist for NextGen OfficeMIPS Resources for NextGen OfficeMy ReportsNextGen Office EHR Certification IDReport Card Export
CMS/QPP Resources
CMS Quality Payment ProgramCMS MIPS OverviewQPP Resource Library
Contact QPP
Call 1-866-288-8292, Monday through Friday, 8:00 AM-8:00 PM ET
E-mail QPP@cms.hhs.gov



