The auto-post feature automatically posts an insurance payment across one or more claims and performs all adjudication processes.
Open ERA Dashboard
From the Billing menu, select Electronic Remittance Advice (ERA).
Auto-post an ERA
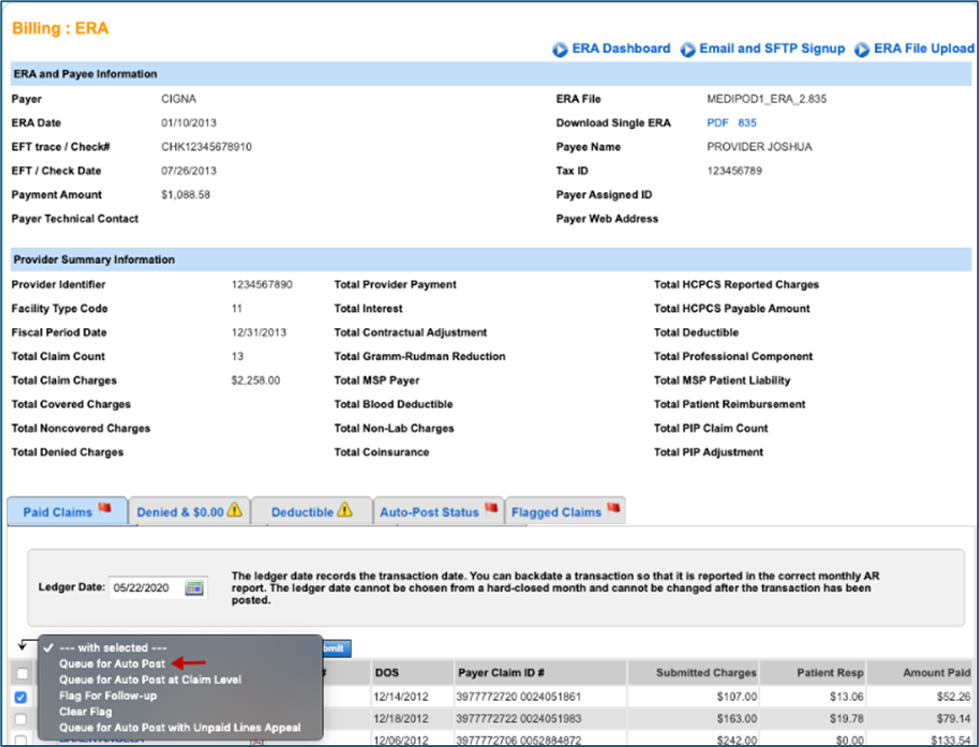
- Click the ERA Date.
- Check for claims in both the Paid Claims and Denied & $0.00 tabs.
- To view the patient's adjudication details prior to auto-posting, click the Patient Name.
- Select the check box next to the patient's name.
- Select one of the following menu options:
- Queue for Auto Post: Most commonly selected. This option auto-posts ERAs at the service-line level. After you finalize the primary claim, you can create secondary claims.
- Queue for Auto Post at Claim Level: This option aggregates everything to one large charge/payment/adjustment. While this works to create primary claims, it may cause additional work when creating secondary claims. We recommend this option if the original queue fails and the status message states "Not enough line level information.”
- Flag for Follow-up: Flags any claims in the ERA for follow-up at a later time.
- Clear Flag: Clears the flag so you can auto-post the claim.
- Queue for Auto Post with Unpaid Lines Appeal: This workflow marks claims that you want to follow up on. Once successfully auto-posted, we move these claims to appealed status in Manage Claims for you to edit and resubmit or follow up with the payer.
You may queue as many ERAs for auto-post as needed. This process may take up to 15 minutes to complete depending on the size of the ERA file.
- Once your claims start to auto-post, a Q appears in the column to the left of the Patient Name.
- When claims process, a green check mark
 (successfully auto-posted) or a red flag
(successfully auto-posted) or a red flag  (failed auto-post) appears.
(failed auto-post) appears. - If at least one claim in the ERA successfully auto-posts, then the check will be successfully posted in the system. If a flag appears, you may need to do some follow up on that claim.
Note: If an ERA is flagged, it cannot be auto-posted. Clear the flag to reattempt.
- Navigate back to the ERA and click the Auto-Post Status tab to view the auto-post status. The reason the claim was flagged is under Status.
ERA Rejections
An auto-post can fail for a number of reasons. When the auto-post fails, the claim and ERA are flagged for follow-up. Below are two possible rejection messages along with the rejection reasons.
Need to Post Manually
- Payment is not balanced
- Claim is not in system
- Service line of claim does not match service line of ERA
- Not enough line-level information: Can attempt a claim-level auto-post
Claim Payer ID Does Not Match ERA Payer ID
The issue occurs when the ERA payer ID does not match the claim payer ID that the claim was submitted to. This error occurs for both paper and electronic claims. There is a specific claim payer ID that is used for these types of claims.
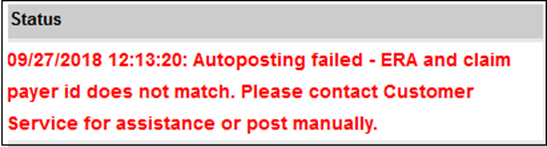
Contact Client Support to have the ERA payer ID matched to the claim payer ID. After the payer is matched, you can reattempt the auto-post on the same day.
Note: When reattempting an auto-post for a flagged claim, you must first clear the flag.
See Also:
ERA Dashboard
Last Review Date: 12/29/25



