What is the Appropriate Use Criteria Program?
When does the AUC program start?
Does NextGen® Office have a CDSM integration?
Do I have to request this integration?
Which patients' radiology orders require AUC consultations?
Is the provider required to order the radiology test?
Which tests required AUC consultation?
How does the AUC requirement affect ordering radiology tests in NextGen Office EHR?
What is required on the claim?
The Protecting Access to Medicare Act (PAMA) of 2014 established the Appropriate Use Criteria (AUC) Program to increase the rate of appropriate advanced diagnostic imaging services provided to Medicare Part B beneficiaries. Examples of such advanced diagnostic imaging services include:
- Computed tomography (CT)
- Positron emission tomography (PET)
- Nuclear medicine
- Magnetic resonance imaging (MRI)
At the time a provider orders an advanced diagnostic imaging service for a Medicare Part B beneficiary, the ordering provider or their clinical staff proxy will be required to consult a qualified Clinical Decision Support Mechanism (CDSM). CDSMs are electronic portals through which AUC is accessed. The CDSM provides a determination of whether the order adheres to AUC, or if the AUC consulted was not applicable (e.g., no AUC is available to address the patient’s clinical condition). (Source: CMS)
For complete information, refer to CMS's Appropriate Use Criteria Program webpage.
January 1, 2023 (CY 2023)
Starting January 1, 2023, AUC consultations with qualified CDSMs are required to occur along with reporting of consultation information on the furnishing professional and furnishing facility claim for the advanced diagnostic imaging service. Claims that fail to append this information will not be paid. (Source: CMS)
CY 2021 and CY 2022 are educational and operations testing periods. Providers should this time to learn and test for the AUC program. Claims will NOT be denied for failing to include AUC consultation information through 2022.
NextGen® Healthcare has partnered with National Decision Support Company (NDSC). We have integrated their solution (CareSelect) within NextGen Office EHR at the time of ordering advanced imaging to assist you in incorporating this requirement into the radiology ordering workflow.
This integration is available to all users. No user action is required.
Medicare Part B beneficiaries
- In the patient chart, primary insurance is Medicare (in Practice Management, Registration > Insurance Information, Payer Type = Medicare)
- Insurance status is Active and not archived
The ordering provider or their auxiliary personnel can consult an approved CDSM to perform AUC consultation. CMS defines auxiliary personnel as clinical staff under the direction of the ordering professional.
For instructions on how to use the AUC feature when ordering a radiology test, refer to the Consult AUC section in
Radiology Orders.
The AUC consultation process is triggered when:
- The AUC feature is enabled for the practice (all practices are enabled by default)
- Patient's primary insurance payer is Medicare and the insurance status is active
- Diagnosis coding has been selected for the encounter
- An advanced diagnostic imaging service is selected for the patient
At the time you or your clinical staff proxy order an advanced diagnostic imaging service for a Medicare Part B beneficiary, you or your clinical staff proxy are required to perform an AUC consultation, which loads the CareSelect Imaging application. The CareSelect application provides the appropriateness rating for the radiology test ordered for the patient and includes alternative tests and their respective ratings. You can replace your selected test with one of the higher-rated recommendations or continue with the test you selected (you must select a reason for selecting a lower-rated test).
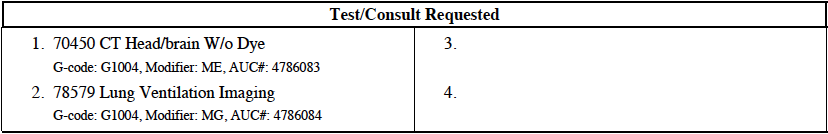
Radiology Order Requisition
The G-code, modifier, and the decision support number for AUC-qualifying and consulted tests are stored in our system and shown on the radiology order requisition form that you can print for, or fax to, the facility that is performing the test and billing the payer for the test.
G-code
G1004 (unique to NDSC (CareSelect)
HCPCS Modifiers
| Modifier | Description |
|---|
| MA | Ordering professional is not required to consult a clinical decision support mechanism due to service being rendered to a patient with a suspected or confirmed emergency medical condition. |
| MB | Ordering professional is not required to consult a clinical decision support mechanism due to the significant hardship exception of insufficient internet access. |
| MC | Ordering professional is not required to consult a clinical decision support mechanism due to the significant hardship exception of electronic health record or clinical decision support mechanism vendor issues. |
| MD | Ordering professional is not required to consult a clinical decision support mechanism due to the significant hardship exception of extreme and uncontrollable circumstances. |
| ME | The order for this service adheres to the appropriate use criteria in the clinical decision support mechanism consulted by the ordering professional. |
| MF | The order for this service does not adhere to the appropriate use criteria in the qualified clinical decision support mechanism consulted by the ordering professional. |
| MG | The order for this service does not have appropriate use criteria in the clinical decision support mechanism consulted by the ordering professional. |
| MH | Unknown if ordering professional consulted a clinical decision support mechanism for this service, related information was not provided to the furnishing professional or provider. |
| QQ | Ordering professional consulted a qualified clinical decision support mechanism. |
CMS Resources



